Pulmonary Embolism
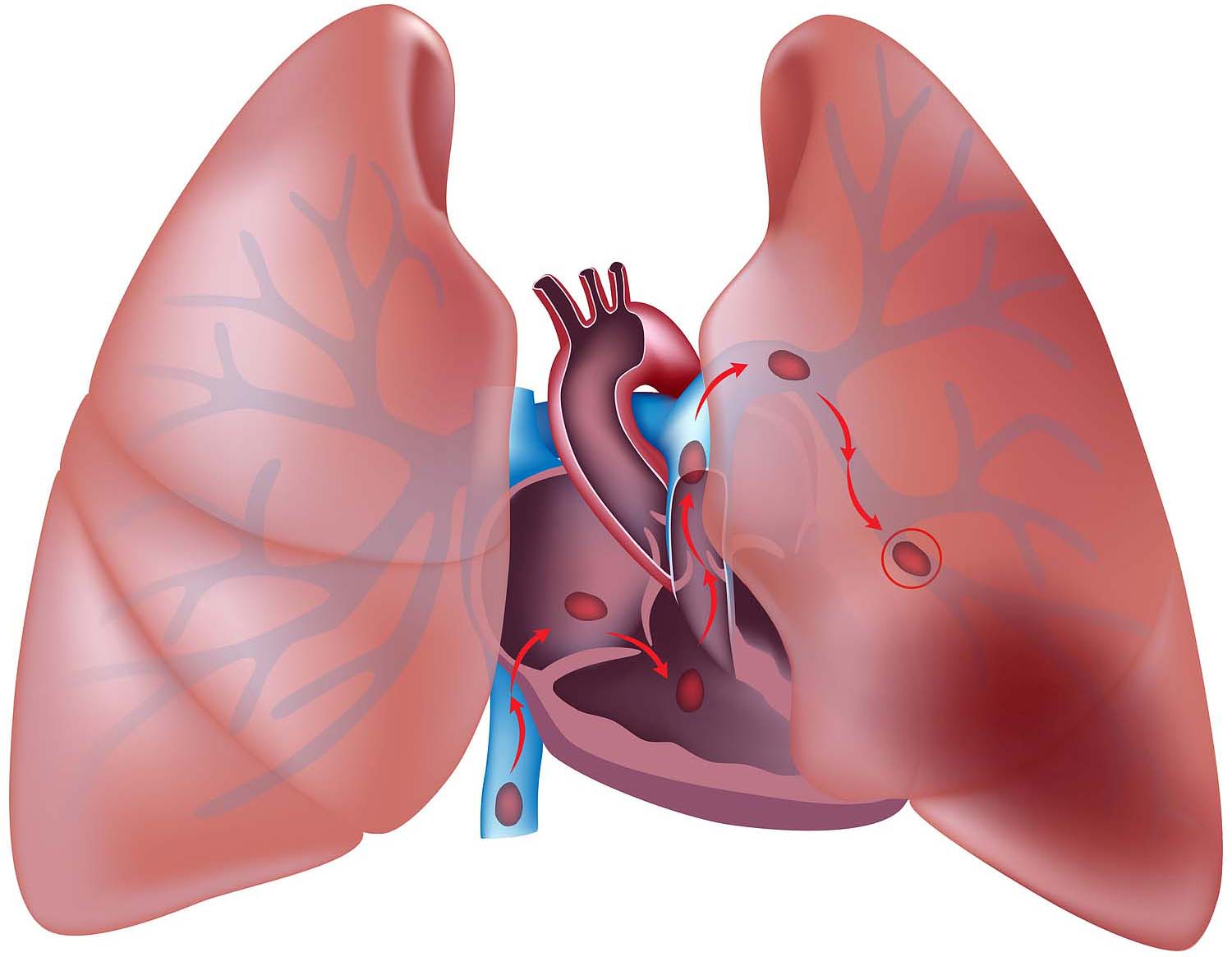
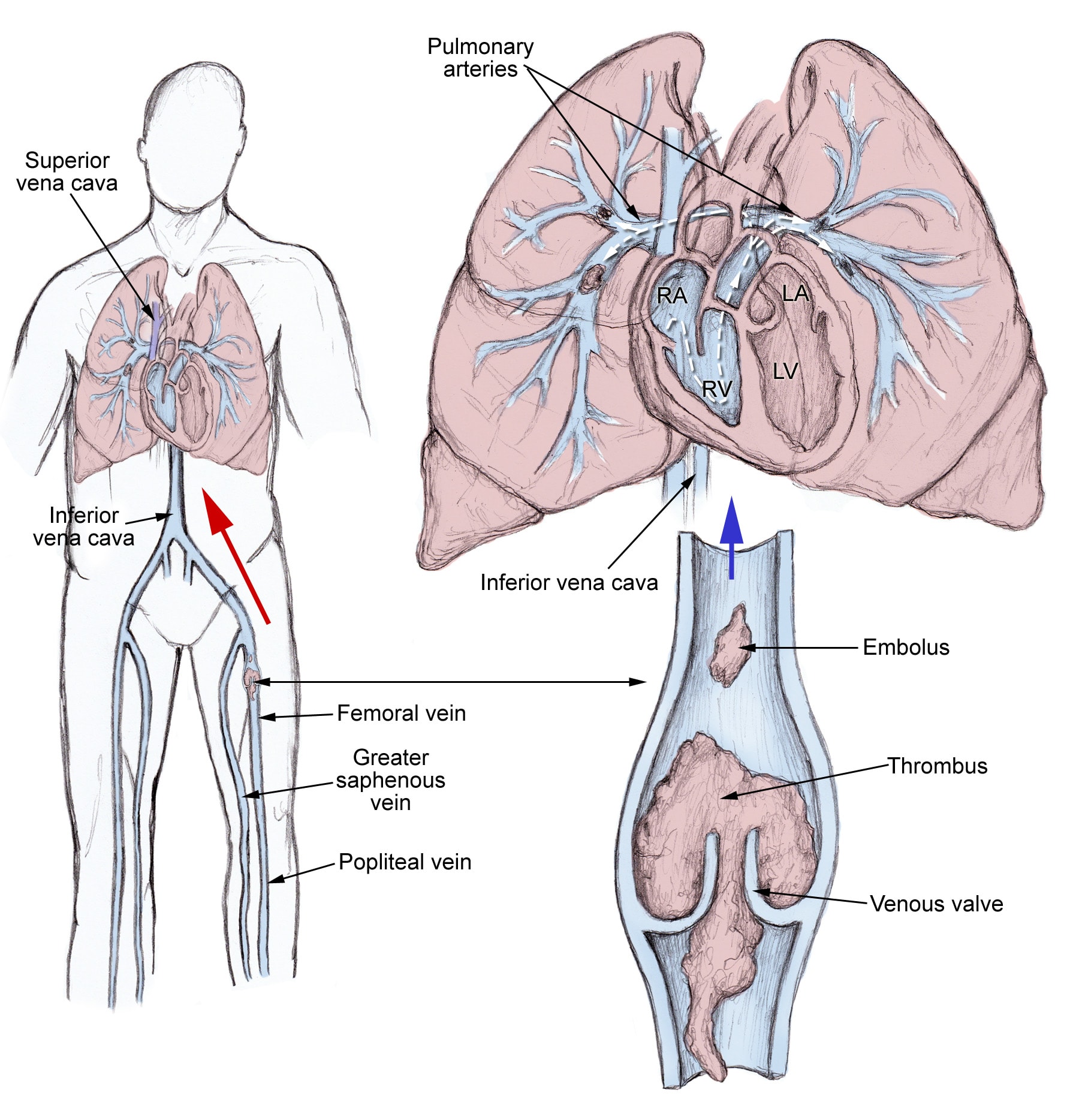
Pulmonary emboli usually arise from thrombi that originate in the deep venous system of the lower extremities; however, they rarely also originate in the pelvic, renal, upper extremity veins, or the right heart chambers (see the image below). After traveling to the lung, large thrombi can lodge at the bifurcation of the main pulmonary artery or the lobar branches and cause hemodynamic compromise.
:Risk Factors
Previous or current DVT
Immobilization
Surgery within the last 3 months
Stroke/paralysis
Central venous instrumentation within the last 3 months
Malignancy
CHF
Autoimmune diseases
Air trav
Thrombophillias
pIn Women
Obesity (BMI ≥29)
Pregnancy
Heavy cigarette smoking (>25 cigarettes per day)
Hypertension
Most Common Symptoms
Dyspnea at rest or with exertion
Pleuritic pain
Cough
pillow orthopnea
Calf or thigh pain
Calf or thigh swelling
Wheezing
Rapid onset of dyspnea
within seconds
within minutes
Most Common Signs
Tachypnea
Tachycardia
Rales
Decreased breath sounds
Accentuated pulmonic component of the second heart sound
Jugular venous distension
Tests and diagnosis
Pulmonary embolism can be difficult to diagnose, especially in people who have underlying heart or lung disease. For that reason, your doctor may order a series of tests to help find the cause of your symptoms. Your doctor may order one or more of the following tests
Blood tests
Your doctor may order a blood test for the clot-dissolving substance D dimer in your blood. High levels may suggest an increased likelihood of blood clots, although D dimer levels may be elevated by many other factors, including recent surgery. In addition, blood tests may be done to determine whether you have an inherited clotting disorder.
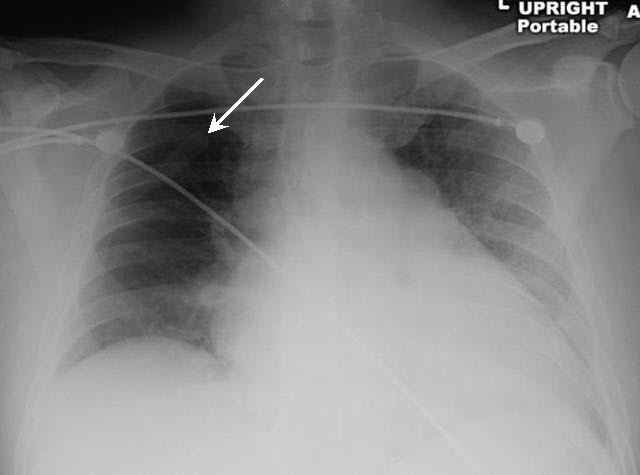
Chest X-ray
This noninvasive test shows images of your heart and lungs on film. Although X-rays can't diagnose pulmonary embolism and may even appear normal when pulmonary embolism exists, they can rule out conditions that mimic the disease.
Ultrasound
A noninvasive "sonar" test known as duplex ultrasonography (sometimes called duplex scan, or compression ultrasonography) uses high-frequency sound waves to check for blood clots in your thigh veins. In this test, your doctor uses a wand-shaped device called a transducer to direct the sound waves to the veins being tested. These waves are then reflected back to the transducer and translated into a moving image by a computer. The absence of the presence of clots reduces the likelihood of DVT. If the upper thigh vessels are clear, the ultrasonography will also scan the veins behind the knee looking for residual clots. If clots are present, treatment likely will be started immediately
CT scan
Regular CT scans take X-rays from many different angles and then combine them to form images showing 2-D "slices" of your internal structures. In a spiral (helical) CT scan, the scanner rotates around your body in a spiral — like the stripe on a candy cane — to create 3-D images. This type of CT can detect abnormalities within the arteries in your lungs with much greater precision, and it's also much faster than are conventional CT scans. In some cases, contrast material is given intravenously during the CT scan to outline the pulmonary arteries
Pulmonary angiogram
This test provides a clear picture of the blood flow in the arteries of your lungs. It's the most accurate way to diagnose pulmonary embolism, but because it requires a high degree of skill to administer and has potentially serious risks, it's usually performed when other tests fail to provide a definitive diagnosis.
In a pulmonary angiogram, a flexible tube (catheter) is inserted into a large vein — usually in your groin — and threaded through into your heart and on into the pulmonary arteries. A special dye is then injected into the catheter, and X-rays are taken as the dye travels along the arteries in your lungs.
One risk of this procedure is a temporary change in your heart rhythm. In addition, the dye may cause kidney damage in people with decreased kidney function.
MRI
MRI scans use radio waves and a powerful magnetic field to produce detailed images of internal structures. Because MRI is expensive, it's usually reserved for pregnant women (to avoid radiation to the fetus) and people whose kidneys may be harmed by dyes used in other tests
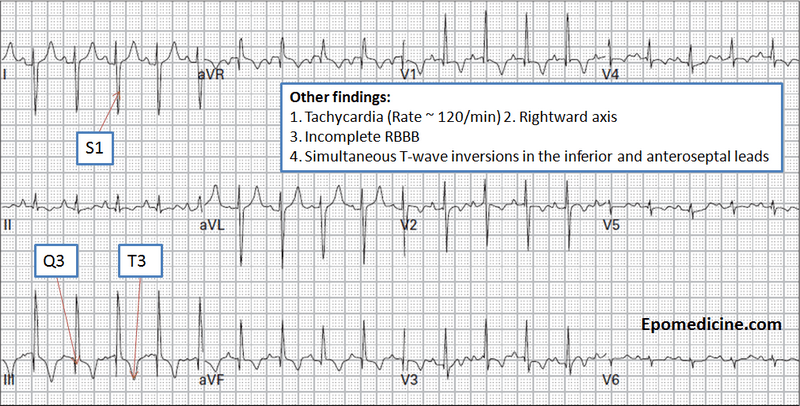
EKG in Pulmonary Embolism
Most commonly sinus tachycardia, with possible nonspecific ST/T wave changes
Only 10% of patients can have the S1Q3T3 so not reliable
Other EKG abnormalities including atrial arrhythmias
right bundle branch block
inferior Q-waves
and precordial Twave
inversion and ST-segment changes, are associated with a poor prognosis
Radiographic Signs – Westermark Sign
Ventilation-Perfusion Scans
Useful if Normal (negative predictive value of 97%
Also useful if High probability (positive predictive value of 85 to 90%
Unfortunately, only diagnostic in 30 to 50% of patients
Treating pulmonary embolism
Anticoagulants
Low molecular weight heparin
Warfarin
Special considerations
Removing the blockage







 رد مع اقتباس
رد مع اقتباس